Pediatric Advanced Life Support on:
[Wikipedia]
[Google]
[Amazon]
Pediatric advanced life support (PALS) is a course offered by the
 PALS builds upon AHA's Pediatric
PALS builds upon AHA's Pediatric
AHA's Pediatric BLS Algorithms
for single and ≥ 2 person rescuer. The most essential component of BLS and PALS cardiac arrest care is high quality cardiopulmonary resuscitation (CPR). CPR should begin with a check for responsiveness, getting help, and activating the emergency response system. After this, the provider should assess for breathing and a pulse ( brachial pulse in infant and
American Heart Association
The American Heart Association (AHA) is a nonprofit organization in the United States that funds cardiovascular medical research, educates consumers on healthy living and fosters appropriate cardiac care in an effort to reduce disability and death ...
(AHA) for health care providers who take care of children and infants in the emergency room
An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of pati ...
, critical care and intensive care unit
220px, Intensive care unit
An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensiv ...
s in the hospital, and out of hospital ( emergency medical services (EMS)). The course teaches healthcare providers how to assess injured and sick children and recognize and treat respiratory distress/failure, shock, cardiac arrest, and arrhythmias.
Basic Life Support (BLS)
 PALS builds upon AHA's Pediatric
PALS builds upon AHA's Pediatric Basic Life Support
Basic life support (BLS) is a level of medical care which is used for patients with life-threatening illnesses or injuries until they can be given full medical care by advanced life support providers (paramedics, nurses, physicians). It can be pr ...
(BLS). Providers should follow thAHA's Pediatric BLS Algorithms
for single and ≥ 2 person rescuer. The most essential component of BLS and PALS cardiac arrest care is high quality cardiopulmonary resuscitation (CPR). CPR should begin with a check for responsiveness, getting help, and activating the emergency response system. After this, the provider should assess for breathing and a pulse ( brachial pulse in infant and
carotid pulse
In anatomy, the left and right common carotid arteries (carotids) (Entry "carotid"
in
If no pulse and no breathing or only gasping, start CPR. CPR consists of chest compressions followed by rescue breaths - for single rescuer do 30 compressions and 2 breaths (30:2), for > 2 rescuers do 15 compressions and 2 breaths (15:2). The rate of chest compressions should be 100-120 compressions/min and depth should be 1.5 inches for infants and 2 inches for children. Chest compressions differ between infants and children. For infants, chest compressions can be done with the two-fingers technique (single rescuer) or two-thumbs encircling hands technique (2 rescuer). In the two-fingers technique, the provider uses their index and middle finger to press down on the infant's If help hasn't arrived after 2 minutes, the provider should call for help again and get an automatic external defibrillator (AED). Once help and the AED arrives, the provider should place the AED pads on the child, making sure to not disrupt chest compressions. The AED will let the provider know if the child has a shockable
If help hasn't arrived after 2 minutes, the provider should call for help again and get an automatic external defibrillator (AED). Once help and the AED arrives, the provider should place the AED pads on the child, making sure to not disrupt chest compressions. The AED will let the provider know if the child has a shockable
 Breathing
* monitor oxygen saturation with a pulse ox
* give supplemental oxygen
* give inhaled medications (e.g.,
Breathing
* monitor oxygen saturation with a pulse ox
* give supplemental oxygen
* give inhaled medications (e.g.,
 Advanced airways may be necessary if the child can't maintain their airway on their own and isn't responding to other methods of ventilation and oxygenation. Advanced airways use medical equipment to allow for open airways and ease of ventilation and medication delivery. Types of advanced airways include supraglottic devices (devices that lie above the
Advanced airways may be necessary if the child can't maintain their airway on their own and isn't responding to other methods of ventilation and oxygenation. Advanced airways use medical equipment to allow for open airways and ease of ventilation and medication delivery. Types of advanced airways include supraglottic devices (devices that lie above the
 The severity of shock is typically based on
The severity of shock is typically based on

 Signs of cardiac arrest include no pulse (within 10 seconds), no breathing or only gasping, and unresponsiveness. As mentioned above, cardiac arrest in kids is mainly a result of respiratory failure and shock, so providers need to treat those conditions quickly and be on the look out for signs of cardiac arrest. Because cardiac arrest can also be caused by arrhythmias, providers should get Electrocardiography, ECGs of these patients. The 4 main cardiac arrest rhythms are Ventricular fibrillation, ventricular fibrillation (VF), pulseless ventricular tachycardia (pVT), asystole, and Pulseless electrical activity, pulseless electrical activity (PEA).
Signs of cardiac arrest include no pulse (within 10 seconds), no breathing or only gasping, and unresponsiveness. As mentioned above, cardiac arrest in kids is mainly a result of respiratory failure and shock, so providers need to treat those conditions quickly and be on the look out for signs of cardiac arrest. Because cardiac arrest can also be caused by arrhythmias, providers should get Electrocardiography, ECGs of these patients. The 4 main cardiac arrest rhythms are Ventricular fibrillation, ventricular fibrillation (VF), pulseless ventricular tachycardia (pVT), asystole, and Pulseless electrical activity, pulseless electrical activity (PEA).
 * Ventricular fibrillation, ventricular fibrillation (VF): disorganized and rapid quivering of the ventricles
* pulseless ventricular tachycardia (pVT): organized wide QRS complexes with no pulse
* asystole: no cardiac electrical activity, ECG shows a flat line
* Ventricular fibrillation, ventricular fibrillation (VF): disorganized and rapid quivering of the ventricles
* pulseless ventricular tachycardia (pVT): organized wide QRS complexes with no pulse
* asystole: no cardiac electrical activity, ECG shows a flat line * Pulseless electrical activity, pulseless electrical activity (PEA): no pulses but ECG shows organized electrical activity (not VF or asystole); not a specific rhythm
* Pulseless electrical activity, pulseless electrical activity (PEA): no pulses but ECG shows organized electrical activity (not VF or asystole); not a specific rhythm
 Treatment of pediatric cardiac arrest follows the American Heart Association's (AHA) Pediatric Cardiac Arrest Algorithm. The goals of treatment are to obtain Return of spontaneous circulation, return of spontaneous circulation (ROSC), meaning that the heart starts working on its own.
Treatment of pediatric cardiac arrest follows the American Heart Association's (AHA) Pediatric Cardiac Arrest Algorithm. The goals of treatment are to obtain Return of spontaneous circulation, return of spontaneous circulation (ROSC), meaning that the heart starts working on its own.
 Once cardiac arrest is recognized, high quality
Once cardiac arrest is recognized, high quality  Once the monitor/defibrillator is connected, the provider should assess the heart rhythm. Of the 4 cardiac arrest rhythms, Ventricular fibrillation, VF and Pulseless ventricular tachycardia, pVT are shockable rhythms and asystole and Pulseless electrical activity, PEA are unshockable rhythms. Shockable rhythms are rhythms that can improve with a shock and thus, should receive a shock. Unshockable rhythms are rhythms that won't improve with a shock and thus, should NOT receive a shock. The monitor/defibrillator will either tell the providers if the rhythm is shockable (Automated external defibrillator, automated external defibrillators (AED)) or the providers will be able to read the ECG and determine for themselves if the rhythm is shockable (manual defibrillators). If shockable, give a shock then resume CPR. If not shockable, continue CPR, give epinephrine, and consider an advanced airway.
After every 2 minutes of giving CPR the provider should reassess the patient's heart rhythm to see if it is shockable or unshockable, and give a shock if it is shockable. This 2 minute cycle of CPR and rhythm assessment should continue until it is determined by the providers that further management is unlikely to save the patient. For patients with shockable rhythms who haven't achieved ROSC, providers can give epinephrine after 2 shocks and amiodarone or lidocaine after 3 shocks. Throughout CPR and rhythm assessments, the providers should be treating any suspected reversible causes of cardiac arrest (H's and T's listed above).
Defibrillations/shocks
* first shock should be 2 J/kg
* second shock should be 4 J/kg
* all other shocks should be ≥ 4 J/kg with max of 10 J/kg
Medicines that can be given during treatment of cardiac arrest are listed below. The doses listed below are for IV/IO medicationa. Medications via endotracheal tube (ET) are often given at higher doses.
*
Once the monitor/defibrillator is connected, the provider should assess the heart rhythm. Of the 4 cardiac arrest rhythms, Ventricular fibrillation, VF and Pulseless ventricular tachycardia, pVT are shockable rhythms and asystole and Pulseless electrical activity, PEA are unshockable rhythms. Shockable rhythms are rhythms that can improve with a shock and thus, should receive a shock. Unshockable rhythms are rhythms that won't improve with a shock and thus, should NOT receive a shock. The monitor/defibrillator will either tell the providers if the rhythm is shockable (Automated external defibrillator, automated external defibrillators (AED)) or the providers will be able to read the ECG and determine for themselves if the rhythm is shockable (manual defibrillators). If shockable, give a shock then resume CPR. If not shockable, continue CPR, give epinephrine, and consider an advanced airway.
After every 2 minutes of giving CPR the provider should reassess the patient's heart rhythm to see if it is shockable or unshockable, and give a shock if it is shockable. This 2 minute cycle of CPR and rhythm assessment should continue until it is determined by the providers that further management is unlikely to save the patient. For patients with shockable rhythms who haven't achieved ROSC, providers can give epinephrine after 2 shocks and amiodarone or lidocaine after 3 shocks. Throughout CPR and rhythm assessments, the providers should be treating any suspected reversible causes of cardiac arrest (H's and T's listed above).
Defibrillations/shocks
* first shock should be 2 J/kg
* second shock should be 4 J/kg
* all other shocks should be ≥ 4 J/kg with max of 10 J/kg
Medicines that can be given during treatment of cardiac arrest are listed below. The doses listed below are for IV/IO medicationa. Medications via endotracheal tube (ET) are often given at higher doses.
*
 Types of bradyarrhythmias
* sinus bradycardia: normal rhythm, slow rate
* atrioventricular block
** First-degree atrioventricular block, first degree: prolonged PR interval (> 0.20 seconds)
** Second-degree atrioventricular block, second degree
*** mobitz type I (wenckebach): progressive lengthening of PR interval then dropped beat (p wave with no QRS)
*** mobitz type II: equal PR intervals with intermittent dropped beats (p wave with no QRS)
** Third-degree atrioventricular block, third degree: complete dissociation between P wave (electrocardiography), p wave and QRS complex, atria and ventricles are beating independent of one another
Types of bradyarrhythmias
* sinus bradycardia: normal rhythm, slow rate
* atrioventricular block
** First-degree atrioventricular block, first degree: prolonged PR interval (> 0.20 seconds)
** Second-degree atrioventricular block, second degree
*** mobitz type I (wenckebach): progressive lengthening of PR interval then dropped beat (p wave with no QRS)
*** mobitz type II: equal PR intervals with intermittent dropped beats (p wave with no QRS)
** Third-degree atrioventricular block, third degree: complete dissociation between P wave (electrocardiography), p wave and QRS complex, atria and ventricles are beating independent of one another
 sinus tachycardia: normal rhythm (normal p waves), fast rate, heart rate usually < 220 bpm (beats per minute) in infants and < 180 bpm in kids
* Supraventricular tachycardia, supraventricular tachycardia (SVT): abnormal rhythm (abnormal p waves), fast rate, originates above the ventricles, heart rate usually > 220 bpm in infants and > 180 bpm in kids, narrow QRS complex, QRS (< 0.09 seconds)
* Ventricular tachycardia, ventricular tachycardia (VT): fast rate, originates in the ventricles, wide QRS (> 0.09 seconds)
sinus tachycardia: normal rhythm (normal p waves), fast rate, heart rate usually < 220 bpm (beats per minute) in infants and < 180 bpm in kids
* Supraventricular tachycardia, supraventricular tachycardia (SVT): abnormal rhythm (abnormal p waves), fast rate, originates above the ventricles, heart rate usually > 220 bpm in infants and > 180 bpm in kids, narrow QRS complex, QRS (< 0.09 seconds)
* Ventricular tachycardia, ventricular tachycardia (VT): fast rate, originates in the ventricles, wide QRS (> 0.09 seconds)
American Heart Association
Pediatric Advanced Life Support Course -- PALS
{{Emergency medicine Medical credentials Emergency medicine courses Emergency life support Pediatrics
in
If no pulse and no breathing or only gasping, start CPR. CPR consists of chest compressions followed by rescue breaths - for single rescuer do 30 compressions and 2 breaths (30:2), for > 2 rescuers do 15 compressions and 2 breaths (15:2). The rate of chest compressions should be 100-120 compressions/min and depth should be 1.5 inches for infants and 2 inches for children. Chest compressions differ between infants and children. For infants, chest compressions can be done with the two-fingers technique (single rescuer) or two-thumbs encircling hands technique (2 rescuer). In the two-fingers technique, the provider uses their index and middle finger to press down on the infant's
sternum
The sternum or breastbone is a long flat bone located in the central part of the chest. It connects to the ribs via cartilage and forms the front of the rib cage, thus helping to protect the heart, lungs, and major blood vessels from injury. Sh ...
, below the nipples. In the two-thumb encircling hands technique, the provider's hands should wrap around the chest with both thumbs pressing down on the infant's sternum. For children, chest compressions should be done with the provider placing the heel of one hand over the child's lower chest and pressing down while keeping their arms straightened at the elbow.
 If help hasn't arrived after 2 minutes, the provider should call for help again and get an automatic external defibrillator (AED). Once help and the AED arrives, the provider should place the AED pads on the child, making sure to not disrupt chest compressions. The AED will let the provider know if the child has a shockable
If help hasn't arrived after 2 minutes, the provider should call for help again and get an automatic external defibrillator (AED). Once help and the AED arrives, the provider should place the AED pads on the child, making sure to not disrupt chest compressions. The AED will let the provider know if the child has a shockable heart rhythm
The cardiac conduction system (CCS) (also called the electrical conduction system of the heart) transmits the signals generated by the sinoatrial node – the heart's pacemaker, to cause the heart muscle to contract, and pump blood through the ...
. If shockable, give a shock
Shock may refer to:
Common uses Collective noun
*Shock, a historic commercial term for a group of 60, see English numerals#Special names
* Stook, or shock of grain, stacked sheaves
Healthcare
* Shock (circulatory), circulatory medical emergen ...
and then immediately resume CPR.
Assessment
PALS teaches a systematic assessment approach so that the health care provider can quickly identify any life-threatening conditions and treat them. The PALS systematic approach algorithm begins with a quick initial assessment followed by checking for responsiveness, pulse, and breathing. If the child has no pulse and isn't breathing, startCPR
Cardiopulmonary resuscitation (CPR) is an emergency procedure consisting of chest compressions often combined with artificial ventilation in an effort to manually preserve intact brain function until further measures are taken to restore sponta ...
. If the child has a pulse but isn't breathing, provide ventilation
Ventilation may refer to:
* Ventilation (physiology), the movement of air between the environment and the lungs via inhalation and exhalation
** Mechanical ventilation, in medicine, using artificial methods to assist breathing
*** Ventilator, a m ...
and give oxygen (when possible). Once it has been established that the child has a pulse, is breathing, and doesn't require immediate life saving treatment, the provider will begin their primary assessment followed by a secondary assessment and further diagnostic workup. Continuous reassessments should be done to reassess for life-threatening conditions.
Initial assessment
The initial assessment is meant to be a very quick assessment performed within the first few seconds of interacting with a child and it utilizes the acronym ABC - appearance, breathing, and color. The provider will assess appearance (level of consciousness and responsiveness, speaking or crying), breathing (breathing or not breathing, increased work of breathing, abnormal breath sounds), and color (pale, mottled,cyanotic
Cyanosis is the change of body tissue color to a bluish-purple hue as a result of having decreased amounts of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Body tissues that show cyanosis are usually in locations ...
, bleeding).
Primary assessment
The primary assessment uses the acronym ABCDE - airway, breathing, circulation, disability, exposure. Airway - assess airway patency (open/patent, unobstructed vs obstructed) and if the patient will need assistance maintaining their airway Breathing - assess respiratory rate, respiratory effort, lung sounds, airway sounds, chest movement,oxygen saturation
Oxygen saturation (symbol SO2) is a relative measure of the concentration of oxygen that is dissolved or carried in a given medium as a proportion of the maximal concentration that can be dissolved in that medium at the given temperature. It ca ...
via pulse oximetry
Pulse oximetry is a noninvasive method for monitoring a person's oxygen saturation. Peripheral oxygen saturation (SpO2) readings are typically within 2% accuracy (within 4% accuracy in 95% of cases) of the more accurate (and invasive) reading of ...
Circulation - assess heart rate, heart rhythm, pulses, skin color, skin temperature, capillary refill time
Capillary refill time (CRT) is defined as the time taken for color to return to an external capillary bed after pressure is applied to cause Blanch (medical), blanching. It can be measured by holding a hand higher than heart-level and pressing th ...
, blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" r ...
Disability - assess neurological function with AVPU pediatric response scale (alert, voice, painful, unresponsive), pediatric Glasgow coma scale
The Glasgow Coma Scale (GCS) is a clinical scale used to reliably measure a person's level of consciousness after a brain injury.
The GCS assesses a person based on their ability to perform eye movements, speak, and move their body. These thre ...
(eye opening, motor response, verbal response), pupil response to light (normal, pinpoint, dilated, unilateral dilated), blood glucose test (low blood sugar/ hypoglycemia
Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose belo ...
can cause altered mental status
An altered level of consciousness is any measure of arousal other than normal. Level of consciousness (LOC) is a measurement of a person's arousability and responsiveness to stimuli from the environment.
A mildly depressed level of consciousne ...
)
Exposure - assess temperature/ fever, signs of trauma (cuts, bleeding, bruises, burns, etc.), skin (petechia
A petechia () is a small red or purple spot (≤4 mm in diameter) that can appear on the skin, conjunctiva, retina, and Mucous membrane, mucous membranes which is caused by haemorrhage of capillaries. The word is derived from Italian , 'freckle,' ...
e, purpura
Purpura () is a condition of red or purple discolored spots on the skin that do not blanch on applying pressure. The spots are caused by bleeding underneath the skin secondary to platelet disorders, vascular disorders, coagulation disorders, ...
, etc.)
Secondary assessment
Once the primary assessment is completed, the provider can do a secondary assessment which consists of a completephysical exam
In a physical examination, medical examination, or clinical examination, a medical practitioner examines a patient for any possible medical signs or symptoms of a medical condition. It generally consists of a series of questions about the patie ...
and focused medical history
The medical history, case history, or anamnesis (from Greek: ἀνά, ''aná'', "open", and μνήσις, ''mnesis'', "memory") of a patient is information gained by a physician by asking specific questions, either to the patient or to other peo ...
. The information asked in the medical history uses the acronym SAMPLE - signs and symptoms
Signs and symptoms are the observed or detectable signs, and experienced symptoms of an illness, injury, or condition. A sign for example may be a higher or lower temperature than normal, raised or lowered blood pressure or an abnormality showin ...
, allergies, medications (prescribed, over the counter, vitamins, herbal), past medical history (any medical problems, prior surgeries), last meal (helpful information to know because it can affect when a child can have surgery or receive anesthesia
Anesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia (relief from or prevention of pain), paralysis (muscle relaxation), ...
), events (onset of illness and events leading up to illness).
Parts of the history that are especially important for children include asking about medications that the child could have gotten into (e.g., if a pill fell on the floor or an unlocked medicine cabinet), history of prematurity, birth history, and immunizations
Immunization, or immunisation, is the process by which an individual's immune system becomes fortified against an infectious agent (known as the immunogen).
When this system is exposed to molecules that are foreign to the body, called ''non-sel ...
.
Respiratory distress and failure
Providers must be able to identify respiratory problems that are easily treatable (e.g., treated with oxygen, suctioning/ clearing airway, albuterocardiac arrest
Cardiac arrest is when the heart suddenly and unexpectedly stops beating. It is a medical emergency that, without immediate medical intervention, will result in sudden cardiac death within minutes. Cardiopulmonary resuscitation (CPR) and possib ...
. Once respiratory complaints have progressed to cardiac arrest
Cardiac arrest is when the heart suddenly and unexpectedly stops beating. It is a medical emergency that, without immediate medical intervention, will result in sudden cardiac death within minutes. Cardiopulmonary resuscitation (CPR) and possib ...
, death and neurological damage are more likely to occur. For this reason, providers should aim to identify and treat respiratory conditions before they progress and worsen.
Recognition
Signs and symptoms
Common signs of respiratory distress * increased work of breathing * nasal flaring (nostrils widening during breathing) * accessory muscle use (using muscles other than the diaphragm andintercostal muscles
Intercostal muscles are many different groups of muscles that run between the ribs, and help form and move the chest wall. The intercostal muscles are mainly involved in the mechanical aspect of breathing by helping expand and shrink the size ...
during breathing (e.g., sternocleidomastoid
The sternocleidomastoid muscle is one of the largest and most superficial cervical muscles. The primary actions of the muscle are rotation of the head to the opposite side and flexion of the neck. The sternocleidomastoid is innervated by the access ...
))
* retractions (collapse of parts of the chest during breathing) (e.g., suprasternal, substernal, sternal, intercostal, subcostal, supraclavicular)
* head bobbing (in infants)
* grunting
* tachypnea
Tachypnea, also spelt tachypnoea, is a respiratory rate greater than normal, resulting in abnormally rapid and shallow breathing.
In adult humans at rest, any respiratory rate of 1220 per minute is considered clinically normal, with tachypnea be ...
(too fast breathing)
* pallor (pale skin)
* tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal (su ...
(fast heart rate)
* agitation and anxiety
Respiratory distress can progress and worsen to respiratory failure. Signs of respiratory failure include the following
* decreased work of breathing
* eventual pauses in or altogether stopping breathing (apnea)
* bradypnea
Bradypnea is abnormally slow breathing. The respiratory rate at which bradypnea is diagnosed depends on the age of the person, with the limit higher during childhood.
Age ranges
* Age 0–1 year < 30 breaths per minute
* Age 1–3 years < 25 br ...
(too slow breathing)
* decreased or absent air movement
* abnormal breath sounds
* cyanosis
Cyanosis is the change of body tissue color to a bluish-purple hue as a result of having decreased amounts of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Body tissues that show cyanosis are usually in locations ...
(blue skin)
* exhaustion and unresponsiveness
* can't speak or cough
Types of respiratory problems
* upper airway obstruction - e.g.,croup
Croup, also known as laryngotracheobronchitis, is a type of respiratory infection that is usually caused by a virus. The infection leads to swelling inside the trachea, which interferes with normal breathing and produces the classic symptoms o ...
, epiglottitis
Epiglottitis is the inflammation of the epiglottis—the flap at the base of the tongue that prevents food entering the trachea (windpipe). Symptoms are usually rapid in onset and include trouble swallowing which can result in drooling, changes t ...
, foreign body aspiration
Foreign body aspiration occurs when a foreign body enters the airway which can cause difficulty breathing or choking. Objects may reach the respiratory tract and the digestive tract from the mouth and nose, but when an object enters the respiratory ...
, anaphylaxis
Anaphylaxis is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of use of emergency medication on site. It typically causes more than one of the follow ...
, retropharyngeal abscess
Retropharyngeal abscess (RPA) is an abscess located in the tissues in the back of the throat behind the posterior pharyngeal wall (the retropharyngeal space). Because RPAs typically occur in deep tissue, they are difficult to diagnose by physical ...
, enlarged/swollen tonsil
The tonsils are a set of lymphoid organs facing into the aerodigestive tract, which is known as Waldeyer's tonsillar ring and consists of the adenoid tonsil, two tubal tonsils, two palatine tonsils, and the lingual tonsils. These organs play an ...
s
* lower airway obstruction - e.g., asthma
Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, cou ...
, bronchiolitis
Bronchiolitis is inflammation of the small airways in the lungs. Acute bronchiolitis is due to a viral infection usually affecting children younger than two years of age. Symptoms may include fever, cough, runny nose, wheezing, and breathing ...
* lung tissue disease - e.g., pneumonia
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity ...
, pneumonitis
Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris (e.g., animal dander), aspiration, herbicides ...
, pulmonary edema
Pulmonary edema, also known as pulmonary congestion, is excessive edema, liquid accumulation in the parenchyma, tissue and pulmonary alveolus, air spaces (usually alveoli) of the lungs. It leads to impaired gas exchange and may cause hypoxemia an ...
* disordered control of breathing - often described as "breathing funny"; e.g., seizure
An epileptic seizure, informally known as a seizure, is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with los ...
, overdose
A drug overdose (overdose or OD) is the ingestion or application of a drug or other substance in quantities much greater than are recommended.
, trauma, coma
A coma is a deep state of prolonged unconsciousness in which a person cannot be awakened, fails to respond normally to painful stimuli, light, or sound, lacks a normal wake-sleep cycle and does not initiate voluntary actions. Coma patients exhi ...
, neuromuscular disease
A neuromuscular disease is any disease affecting the peripheral nervous system (PNS), the neuromuscular junction, or skeletal muscle, all of which are components of the motor unit. Damage to any of these structures can cause muscle atrophy and w ...
s
Management
Initial management
The initial management for respiratory distress uses the acronym ABC - airway, breathing, circulation. Airway * support the airway by making sure that it is open/patent (child can do this on their own or provider may have to open airway with head tilt-chin lift orjaw thrust
The jaw-thrust maneuver is a first aid and medical procedure used to prevent the tongue from obstructing the upper airways. This maneuver and the head-tilt/chin-lift maneuver are two of the main tools of basic airway management, and they are ...
(if suspected cervical spine injury))
* clear the airway as needed (e.g., suctioning mucus/secretions in nose and throat, removing foreign bodies, etc.)
* consider adding airway adjuncts such as nasopharyngeal airway (NPA) or oropharyngeal airway (OPA) (if no gag reflex)albuterol
Salbutamol, also known as albuterol and sold under the brand name Ventolin among others, is a medication that opens up the medium and large airways in the lungs. It is a short-acting β2 adrenergic receptor agonist which works by causing rel ...
, epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands and ...
) as needed
* manually ventilate as needed (e.g., bag mask ventilation)
* prepare for advanced airway
Circulation
* monitor vitals (e.g., heart rate
Heart rate (or pulse rate) is the frequency of the heartbeat measured by the number of contractions (beats) of the heart per minute (bpm). The heart rate can vary according to the body's physical needs, including the need to absorb oxygen and excr ...
, blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" r ...
)
* establish vascular access (for medications and fluids) as needed
Advanced airways
 Advanced airways may be necessary if the child can't maintain their airway on their own and isn't responding to other methods of ventilation and oxygenation. Advanced airways use medical equipment to allow for open airways and ease of ventilation and medication delivery. Types of advanced airways include supraglottic devices (devices that lie above the
Advanced airways may be necessary if the child can't maintain their airway on their own and isn't responding to other methods of ventilation and oxygenation. Advanced airways use medical equipment to allow for open airways and ease of ventilation and medication delivery. Types of advanced airways include supraglottic devices (devices that lie above the glottis
The glottis is the opening between the vocal folds (the rima glottidis). The glottis is crucial in producing vowels and voiced consonants.
Etymology
From Ancient Greek ''γλωττίς'' (glōttís), derived from ''γλῶττα'' (glôtta), va ...
such as OPA, NPA, laryngeal mask airway
A laryngeal mask airway (LMA), also known as laryngeal mask, is a medical device that keeps a patient's airway open during anaesthesia or while they are unconscious. It is a type of supraglottic airway device. They are most commonly used by anae ...
), infraglottic devices (devices that lie below the glottis and go into the trachea
The trachea, also known as the windpipe, is a Cartilage, cartilaginous tube that connects the larynx to the bronchi of the lungs, allowing the passage of air, and so is present in almost all air-breathing animals with lungs. The trachea extends ...
such as endotracheal tube
A tracheal tube is a catheter that is inserted into the trachea for the primary purpose of establishing and maintaining a patent airway and to ensure the adequate exchange of oxygen and carbon dioxide.
Many different types of tracheal tubes are a ...
(intubation
Intubation (sometimes entubation) is a medical procedure involving the insertion of a tube into the body. Patients are generally anesthetized beforehand. Examples include tracheal intubation, and the balloon tamponade with a Sengstaken-Blakemo ...
)), and surgery (incision below the glottis such as cricothyrotomy
A cricothyrotomy (also called cricothyroidotomy) is an incision made through the skin and cricothyroid membrane to establish a patent airway during certain life-threatening situations, such as airway obstruction by a foreign body, angioedema, or ...
and tracheotomy
Tracheotomy (, ), or tracheostomy, is a surgical airway management procedure which consists of making an incision (cut) on the anterior aspect (front) of the neck and opening a direct airway through an incision in the trachea (windpipe). The ...
). Surgical advanced airways are typically performed intubation and other less invasive methods fail or are contraindicated or when the child will need long term mechanical ventilation
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air ...
.
Intubation
To perform an intubation, the health care provider should be able to perform the steps ofrapid sequence intubation
In advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is ...
(preparation, preoxygenation, pretreatment, paralysis and sedation, positioning, placement of tube, postintubation management).
Further management
Further management should be based on the specific medical condition the child has. For example, if the child is experiencing respiratory distress secondary toasthma
Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, cou ...
, management would include albuterol
Salbutamol, also known as albuterol and sold under the brand name Ventolin among others, is a medication that opens up the medium and large airways in the lungs. It is a short-acting β2 adrenergic receptor agonist which works by causing rel ...
, inhaled corticosteroids
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are involv ...
, supplemental oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements as wel ...
, and more depending upon the severity of the asthma.
Shock
Shock
Shock may refer to:
Common uses Collective noun
*Shock, a historic commercial term for a group of 60, see English numerals#Special names
* Stook, or shock of grain, stacked sheaves
Healthcare
* Shock (circulatory), circulatory medical emergen ...
is defined as inadequate blood flow (perfusion
Perfusion is the passage of fluid through the circulatory system or lymphatic system to an organ or a tissue, usually referring to the delivery of blood to a capillary bed in tissue. Perfusion is measured as the rate at which blood is deliver ...
) in the body, causing tissues and organs to (1) not get enough oxygen and nutrients and (2) have trouble getting rid of toxic products of metabolism (e.g., lactate). It is important to recognize and treat shock as early as possible because the body requires oxygen and nutrients to function and without them, organs can eventually shut down and people can die. Common signs of shock include weak pulses, altered mental status
An altered level of consciousness is any measure of arousal other than normal. Level of consciousness (LOC) is a measurement of a person's arousability and responsiveness to stimuli from the environment.
A mildly depressed level of consciousne ...
, bradycardia
Bradycardia (also sinus bradycardia) is a slow resting heart rate, commonly under 60 beats per minute (BPM) as determined by an electrocardiogram. It is considered to be a normal heart rate during sleep, in young and healthy or elderly adults, a ...
or tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal (su ...
, low urine output, hypotension
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure (the top number) and the dias ...
, and pale, cold skin. Treating shock focuses on increasing blood flow and oxygen delivery to tissues and organs before organs are permanently damaged. This section will discuss the recognition and management of shock.
Recognition
Shock severity
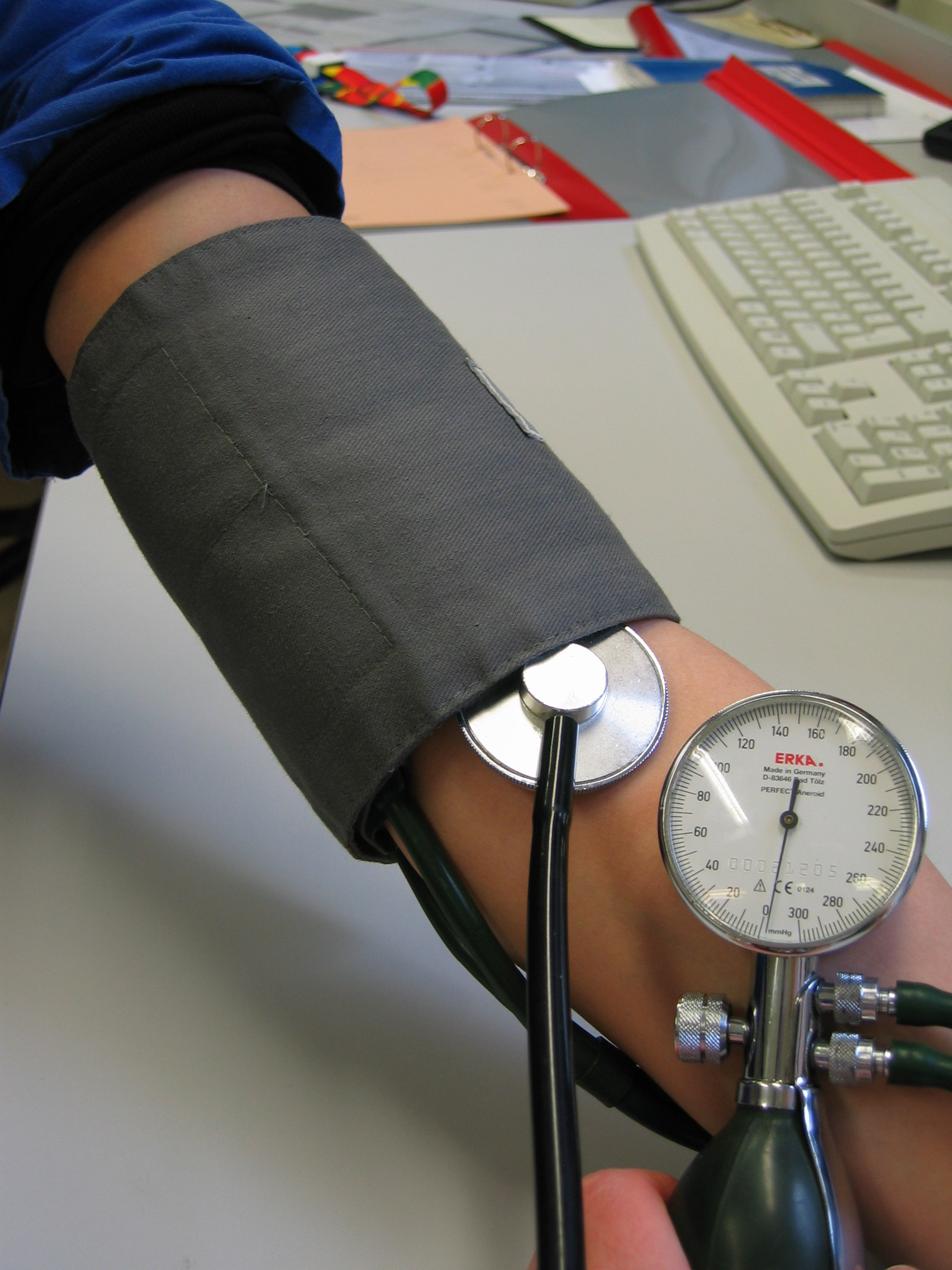
systolic blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" r ...
. For this reason, measuring blood pressure is an important way to assess shock; however, blood pressure machines may not be very accurate if pulses are weak and the arms and legs (where the blood pressure is measured) are poorly perfused.
Compensated shock is when the body is able to compensate through various mechanisms (e.g., raising the heart rate, increasing systemic vascular resistance, and more) to keep the systolic blood pressure in a normal range.
Hypotensive/ decompensated shock is when the body cannot maintain systolic blood pressure in the normal range, and it becomes too low (hypotensive
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure (the top number) and the dias ...
).
Types of shock
There are 4 main types of shock: hypovolemic, distributive, cardiogenic, and obstructive.Hypovolemic shock
Hypovolemic shock
Hypovolemic shock is a form of shock caused by severe hypovolemia (insufficient blood volume or extracellular fluid in the body). It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a ...
is caused by low blood volume (hypovolemia) and is the most common cause of shock in pediatric patients. Common causes of volume loss include diarrhea
Diarrhea, also spelled diarrhoea, is the condition of having at least three loose, liquid, or watery bowel movements each day. It often lasts for a few days and can result in dehydration due to fluid loss. Signs of dehydration often begin wi ...
, vomiting, hemorrhage
Bleeding, hemorrhage, haemorrhage or blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vag ...
, not drinking enough, burns, osmotic diuresis (e.g., diabetic ketoacidosis
Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of diabetes mellitus. Signs and symptoms may include vomiting, abdominal pain, deep gasping breathing, increased urination, weakness, confusion and occasionally loss of ...
), and third space
The human body and even its individual body fluids may be conceptually divided into various fluid compartments, which, although not literally anatomic compartments, do represent a real division in terms of how portions of the body's water, solute ...
losses. Signs of hypovolemic shock are related to the low blood volume and decreased blood flow to extremities (e.g., cold extremities, slow capillary refill
Capillary refill time (CRT) is defined as the time taken for color to return to an external capillary bed after pressure is applied to cause blanching. It can be measured by holding a hand higher than heart-level and pressing the soft pad of a f ...
, and weak distal pulses).
Distributive shock
Distributive shock
Distributive shock is a medical condition in which abnormal distribution of blood flow in the smallest blood vessels results in inadequate supply of blood to the body's tissues and organs. It is one of four categories of shock, a condition where ...
is caused by abnormally distributed blood throughout the body which causes some parts of the body to receive inadequate blood supply. Common causes of distributive shock include sepsis
Sepsis, formerly known as septicemia (septicaemia in British English) or blood poisoning, is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs. This initial stage is follo ...
, anaphylaxis
Anaphylaxis is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of use of emergency medication on site. It typically causes more than one of the follow ...
, and head or spinal cord injury (neurogenic shock
Neurogenic shock is a distributive type of shock resulting in hypotension (low blood pressure), often with bradycardia (slowed heart rate), caused by disruption of autonomic nervous system pathways. It can occur after damage to the central nervou ...
).
* Septic shock is typically caused by an infection or inflammation in the body. Signs of septic shock include fever
Fever, also referred to as pyrexia, is defined as having a body temperature, temperature above the human body temperature, normal range due to an increase in the body's temperature Human body temperature#Fever, set point. There is not a single ...
or hypothermia
Hypothermia is defined as a body core temperature below in humans. Symptoms depend on the temperature. In mild hypothermia, there is shivering and mental confusion. In moderate hypothermia, shivering stops and confusion increases. In severe h ...
, petechia
A petechia () is a small red or purple spot (≤4 mm in diameter) that can appear on the skin, conjunctiva, retina, and Mucous membrane, mucous membranes which is caused by haemorrhage of capillaries. The word is derived from Italian , 'freckle,' ...
, and purpura
Purpura () is a condition of red or purple discolored spots on the skin that do not blanch on applying pressure. The spots are caused by bleeding underneath the skin secondary to platelet disorders, vascular disorders, coagulation disorders, ...
. Lab tests might show leukocytosis or leukopenia, metabolic acidosis with high lactate, and more.
* Anaphylactic shock is caused by an allergen and common signs include facial swelling, throat swelling, hives, Wheeze, wheezing, etc.
Cardiogenic shock
Cardiogenic shock is caused by abnormal heart function or problems within the heart that impair pumping of blood within the heart. Common causes of cardiogenic shock include Congenital heart defect, congenital heart diseases, arrhythmias, myocarditis (inflammation of the heart muscle), cardiomyopathy (impairment of the heart's ability to pump), trauma/injury of the heart, drug or poison toxicity. Common signs include tachycardia, distant pulses, and worsening with giving fluids.Obstructive shock
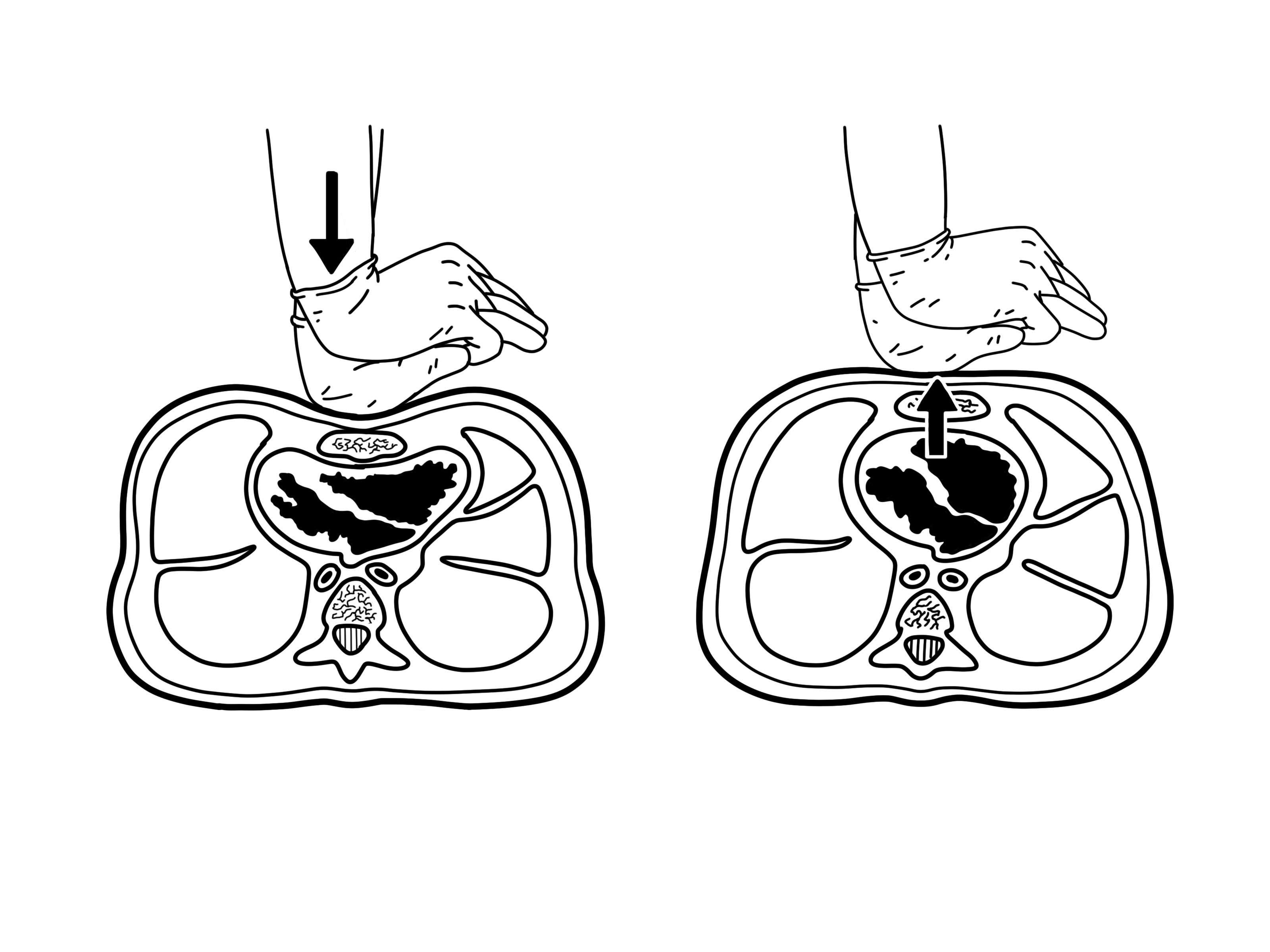
Obstructive shock is caused by disrupted flow of blood to the heart or flow of blood out of the heart. Common causes include Pneumothorax, tension pneumothorax, cardiac tamponade, pulmonary embolism, and ductal dependent congenital heart defects (conditions that worsen when the ductus arteriosus closes after birth) (e.g., hypoplastic left heart syndrome and coarctation of the aorta). * Pneumothorax, Tension pneumothorax: a build up of air in the Pleural cavity, pleural space of the lungs causing compression and collapse of the lung. Common signs include trauma to the chest, Jugular venous distension, distended neck veins, tracheal deviation (away from side of injury), and decreased breath sounds on side of injury. * Cardiac tamponade: a build up of fluid or blood in the space surrounding the heart (Pericardial space, pericardium) causing compression of the heart. Common signs include muffled heart sounds and pulsus paradoxus. * Pulmonary embolism: obstruction of a pulmonary artery or a branch of the pulmonary arteries most commonly by a clot causing blocked flow of blood out of or back into the heart. Children with predispositions to forming clots such as those with sickle cell disease, cancer, Coagulopathy, coagulation disorders, and central venous catheters are more likely to have pulmonary emboli. Common signs include worsening heart and lung function as evidenced by chest pain,tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal (su ...
, shortness of breath, heart failure, and more.
Management
Management of shock should be based on the type of shock. When the type of shock hasn't been identified yet, the provider should start with some initial treatments and labs. All children with suspected shock should receive supplementaloxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements as wel ...
, ventilation if in respiratory distress (via Nasal cannula, nasal canula, High flow nasal cannula, high flow nasal canula, Non-invasive ventilation, noninvasive ventilation, or mechanical ventilation
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air ...
), and treatment for life-threatening conditions. Providers should establish vascular access (Intravenous therapy, intravenous access [2 peripheral Intravenous therapy, IVs with a large caliber needle] and if that isn't possible, Intraosseous infusion, intraosseous access (IO) or Central venous catheter, central venous line). Providers should also obtain initial lab studies including a Blood sugar level, rapid blood glucose, basic metabolic panel (BMP) (measures serum electrolytes, blood urea nitrogen, and creatinine), Lactic acidosis, lactic acid level, complete blood count (CBC), and Urine test strip, urine dipstick.

Fluids
The provider should start crystalloid fluids (Saline (medicine), normal saline or Ringer's lactate solution, lactated Ringers). For compensated shock give 10-20 ml/kg over 5-20 min and for hypotensive shock, give 20 ml/lg over 5-10 min. However, if there are signs that the patient has too much fluid (fluid overload) such as worsening respiratory distress, Jugular venous pressure, jugular venous distention, crackles, hepatomegaly, then fluids should not be given. With continued signs of shock and no signs of fluid overload, kids can continue to receive 10-20 ml/kg of fluids with a max of 60 ml/kg in the first hour. However, if cardiogenic shock is suspected, kids should receive less fluids over a longer time (e.g., 5-10 ml/kg over 15-30 min).Hypovolemic shock
Hypovolemic shock is mainly treated with fluid replacement, as described in the fluids section above. If the hypovolemic shock is caused by a hemorrhage, then the provider should obtain blood type, blood Cross-matching, cross match, and coagulation studies (Prothrombin time, PT, International Normalized Ratio, INR, Partial thromboplastin time, PTT). In hemorrhagic shock, patients should receive blood or blood products if they aren't improving with fluids.Distributive shock
Distributive shock is mainly treated with fluid replacement, as described in the fluids section above, and vasopressors. For those with suspected septic shock, providers should obtain blood culture, urinalysis, urine culture, C-reactive protein, c-reactive protein (CRP) (marker of inflammation), procalcitonin (marker of inflammation), fibrinogen, D-dimer, bilirubin labs, and more. Those in anaphylactic shock should be treated with Epinephrine autoinjector, intramuscular epinephrine.Cardiogenic shock
Cardiogenic shock typically worsens with fluids. Providers should obtain an Electrocardiography, ECG and echocardiogram for patients suspected to have cardiogenic shock. Treatment can include vasopressors, inotropes, and treatment of any arrhythmias.Obstructive shock
Obstructive shock is treated by treating the underlying cause of the shock. Tension pneumothorax is treated with a chest tube and Thoracentesis, needle thoracostomy which allows the air to get out of the pleural space. Cardiac tamponade is treated with pericardiocentesis which removes the fluid from the pericardium and decompresses the heart. Pulmonary embolism is treated with anticoagulants (prevent body from making more clots) and if bad enough, thrombectomy (surgical removal of clots). Ductal dependent congenital heart defects are treated with prostaglandin E1/ alprostadil which keeps the ductus arteriosus open.Cardiac Arrest
Cardiac arrest occurs when the heart stops working and blood stops moving throughout the body. In infants and children, cardiac arrest is typically caused by (1) hypoxic/asphyxial arrest and less commonly by (2) sudden cardiac arrest due to heart problems or arrhythmias. In adults, cardiac arrest is usually caused by heart problems such as acute coronary syndrome. Hypoxic/asphyxial cardiac arrest is a result of progressive respiratory failure and/or shock. For this reason, it is important to treat respiratory failure and shock early so that they don't progress to cardiac arrest. Sudden cardiac arrest is typically caused by arrhythmias such Ventricular fibrillation, ventricular fibrillation (VF) and Ventricular tachycardia, pulseless ventricular tachycardia (pVT). These arrhythmias are more common in kids with hypertrophic cardiomyopathy, cardiac Channelopathy, channelopathies (e.g., long QT syndrome), myocarditis, drugs (e.g., Cocaine intoxication, cocaine, Digoxin toxicity, digoxin), commotio cordis, and anomalous coronary artery. There are many causes of reversible cardiac arrest and the mnemonic "H's and T's" is used to remember these causes.Recognition
 Signs of cardiac arrest include no pulse (within 10 seconds), no breathing or only gasping, and unresponsiveness. As mentioned above, cardiac arrest in kids is mainly a result of respiratory failure and shock, so providers need to treat those conditions quickly and be on the look out for signs of cardiac arrest. Because cardiac arrest can also be caused by arrhythmias, providers should get Electrocardiography, ECGs of these patients. The 4 main cardiac arrest rhythms are Ventricular fibrillation, ventricular fibrillation (VF), pulseless ventricular tachycardia (pVT), asystole, and Pulseless electrical activity, pulseless electrical activity (PEA).
Signs of cardiac arrest include no pulse (within 10 seconds), no breathing or only gasping, and unresponsiveness. As mentioned above, cardiac arrest in kids is mainly a result of respiratory failure and shock, so providers need to treat those conditions quickly and be on the look out for signs of cardiac arrest. Because cardiac arrest can also be caused by arrhythmias, providers should get Electrocardiography, ECGs of these patients. The 4 main cardiac arrest rhythms are Ventricular fibrillation, ventricular fibrillation (VF), pulseless ventricular tachycardia (pVT), asystole, and Pulseless electrical activity, pulseless electrical activity (PEA).
 * Pulseless electrical activity, pulseless electrical activity (PEA): no pulses but ECG shows organized electrical activity (not VF or asystole); not a specific rhythm
* Pulseless electrical activity, pulseless electrical activity (PEA): no pulses but ECG shows organized electrical activity (not VF or asystole); not a specific rhythm
Management
 Treatment of pediatric cardiac arrest follows the American Heart Association's (AHA) Pediatric Cardiac Arrest Algorithm. The goals of treatment are to obtain Return of spontaneous circulation, return of spontaneous circulation (ROSC), meaning that the heart starts working on its own.
Treatment of pediatric cardiac arrest follows the American Heart Association's (AHA) Pediatric Cardiac Arrest Algorithm. The goals of treatment are to obtain Return of spontaneous circulation, return of spontaneous circulation (ROSC), meaning that the heart starts working on its own.
 Once cardiac arrest is recognized, high quality
Once cardiac arrest is recognized, high quality CPR
Cardiopulmonary resuscitation (CPR) is an emergency procedure consisting of chest compressions often combined with artificial ventilation in an effort to manually preserve intact brain function until further measures are taken to restore sponta ...
needs to be started immediately. After starting chest compressions, the provider should (1) give ventilations (via Bag valve mask, bag mask) and oxygen, (2) attach monitor/Defibrillation, defibrillator pads or ECG electrodes to the child so that Defibrillation, defibrillations (aka shocks) can be given if needed, and (3) establish vascular access (IV, IO). Attaching the defibrillator and establishing vascular access should NOT interrupt chest compressions.
 Once the monitor/defibrillator is connected, the provider should assess the heart rhythm. Of the 4 cardiac arrest rhythms, Ventricular fibrillation, VF and Pulseless ventricular tachycardia, pVT are shockable rhythms and asystole and Pulseless electrical activity, PEA are unshockable rhythms. Shockable rhythms are rhythms that can improve with a shock and thus, should receive a shock. Unshockable rhythms are rhythms that won't improve with a shock and thus, should NOT receive a shock. The monitor/defibrillator will either tell the providers if the rhythm is shockable (Automated external defibrillator, automated external defibrillators (AED)) or the providers will be able to read the ECG and determine for themselves if the rhythm is shockable (manual defibrillators). If shockable, give a shock then resume CPR. If not shockable, continue CPR, give epinephrine, and consider an advanced airway.
After every 2 minutes of giving CPR the provider should reassess the patient's heart rhythm to see if it is shockable or unshockable, and give a shock if it is shockable. This 2 minute cycle of CPR and rhythm assessment should continue until it is determined by the providers that further management is unlikely to save the patient. For patients with shockable rhythms who haven't achieved ROSC, providers can give epinephrine after 2 shocks and amiodarone or lidocaine after 3 shocks. Throughout CPR and rhythm assessments, the providers should be treating any suspected reversible causes of cardiac arrest (H's and T's listed above).
Defibrillations/shocks
* first shock should be 2 J/kg
* second shock should be 4 J/kg
* all other shocks should be ≥ 4 J/kg with max of 10 J/kg
Medicines that can be given during treatment of cardiac arrest are listed below. The doses listed below are for IV/IO medicationa. Medications via endotracheal tube (ET) are often given at higher doses.
*
Once the monitor/defibrillator is connected, the provider should assess the heart rhythm. Of the 4 cardiac arrest rhythms, Ventricular fibrillation, VF and Pulseless ventricular tachycardia, pVT are shockable rhythms and asystole and Pulseless electrical activity, PEA are unshockable rhythms. Shockable rhythms are rhythms that can improve with a shock and thus, should receive a shock. Unshockable rhythms are rhythms that won't improve with a shock and thus, should NOT receive a shock. The monitor/defibrillator will either tell the providers if the rhythm is shockable (Automated external defibrillator, automated external defibrillators (AED)) or the providers will be able to read the ECG and determine for themselves if the rhythm is shockable (manual defibrillators). If shockable, give a shock then resume CPR. If not shockable, continue CPR, give epinephrine, and consider an advanced airway.
After every 2 minutes of giving CPR the provider should reassess the patient's heart rhythm to see if it is shockable or unshockable, and give a shock if it is shockable. This 2 minute cycle of CPR and rhythm assessment should continue until it is determined by the providers that further management is unlikely to save the patient. For patients with shockable rhythms who haven't achieved ROSC, providers can give epinephrine after 2 shocks and amiodarone or lidocaine after 3 shocks. Throughout CPR and rhythm assessments, the providers should be treating any suspected reversible causes of cardiac arrest (H's and T's listed above).
Defibrillations/shocks
* first shock should be 2 J/kg
* second shock should be 4 J/kg
* all other shocks should be ≥ 4 J/kg with max of 10 J/kg
Medicines that can be given during treatment of cardiac arrest are listed below. The doses listed below are for IV/IO medicationa. Medications via endotracheal tube (ET) are often given at higher doses.
* epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands and ...
: 0.01 mg/kg every 3–5 minutes with max single dose of 1 mg
* amiodarone: 5 mg/kg initially, can repeat 2 more times (total of 3 doses), max of 300 mg per dose, max 15 mg/kg, given for refractory VF and pVT
* lidocaine: 1 mg/kg initially with continuous infusion of 20-50 mcg/kg/min after, given for refractory VF and pVT
* Magnesium sulfate (medical use), magnesium sulfate: 25–50 mg/kg diluted in 10 ml D5W (5% dextrose) and infused over 1–2 minutes, max 2g per dose, given for pulseless torsades de pointes (a type of ventricular tachycardia)
Arrhythmias
PALS providers should be able to identify and treat different types of abnormal pediatric heart rhythms including Bradycardia, bradyarrhythmias, Tachycardia, tachyarrhythmias, and cardiac arrest rhythms (discussed above). In defining heart rates that are too slow or too fast, it is important to understand the ranges of pediatric heart rates by age. Normal ranges of pediatric heart rates change with age, with heart rates being faster closer to birth and slower closer to adulthood.Bradyarrythmias
Bradycardia is defined as a slow heart rate for a child's age. Bradycardia associated with signs of shock (altered mental status, hypotension, etc.) can be an early warning sign for cardiac arrest. Signs of bradycardia include fatigue, confusion, dizziness, and lightheadedness. Possible causes of bradycardia include Hypoxia (medical), hypoxia,hypothermia
Hypothermia is defined as a body core temperature below in humans. Symptoms depend on the temperature. In mild hypothermia, there is shivering and mental confusion. In moderate hypothermia, shivering stops and confusion increases. In severe h ...
, and certain medications.
 Types of bradyarrhythmias
* sinus bradycardia: normal rhythm, slow rate
* atrioventricular block
** First-degree atrioventricular block, first degree: prolonged PR interval (> 0.20 seconds)
** Second-degree atrioventricular block, second degree
*** mobitz type I (wenckebach): progressive lengthening of PR interval then dropped beat (p wave with no QRS)
*** mobitz type II: equal PR intervals with intermittent dropped beats (p wave with no QRS)
** Third-degree atrioventricular block, third degree: complete dissociation between P wave (electrocardiography), p wave and QRS complex, atria and ventricles are beating independent of one another
Types of bradyarrhythmias
* sinus bradycardia: normal rhythm, slow rate
* atrioventricular block
** First-degree atrioventricular block, first degree: prolonged PR interval (> 0.20 seconds)
** Second-degree atrioventricular block, second degree
*** mobitz type I (wenckebach): progressive lengthening of PR interval then dropped beat (p wave with no QRS)
*** mobitz type II: equal PR intervals with intermittent dropped beats (p wave with no QRS)
** Third-degree atrioventricular block, third degree: complete dissociation between P wave (electrocardiography), p wave and QRS complex, atria and ventricles are beating independent of one another
Management
Providers should follow the AHA's Pediatric Bradycardia With a Pulse Algorithm. As always, provides need to support airway, breathing, and circulation and begin CPR if needed. Bradyarrythmias with signs of shock can be treated with epinephrine and atropine in order to increase heart rate. If medications aren't helping, providers can consider cardiac Pacing technology, pacing. * epinephrine: 0.01 mg/kg every 3–5 minutes * atropine: 0.02 mg/kg, can repeat one time, max dose 0.5 mg, min dose of 0.1 mgTachyarrhythmias
Tachycardia is defined as a fast heart rate for a child's age. Signs of tachycardia are similar to bradycardia but also include palpitations, decreased feeding/eating, and irritability. Tachyarrhythmias are fast abnormal heart rhythms. Types of tachyarrhythmias *Management
Providers should follow the AHA's Pediatric Tachycardia With a Pulse Algorithm. As always, provides need to support airway, breathing, and circulation and begin CPR if needed. Management of tachyarrhythmias depends on if the child is stable or unstable (experiencing cardiopulmonary compromise: signs of shock, hypotension, altered mental status). Unstable tachyarrhythmia is treated with Cardioversion, synchronized cardioversion - initially 0.5-1 J/kg but can increase to 2 J/kg if smaller dose is not working. Stable tachyarrhythmia treatment is subcategorized based on narrow QRS complex, QRS vs. wide QRS. If narrow QRS/ SVT, perform vagal maneuvers and give adenosine. If wide QRS/ VT with regular rhythm and monomorphic QRS, the provider can give adenosine and should consult pediatric cardiology for recommendations. * adenosine: first dose 0.1 mg/kg with max 6 mg, second dose 0.2 mg/kg with max 12 mgCriticism
PETA has criticized the use of animals in PALS training which the organization calls "cruel and unnecessary". PETA says that hundreds of PALS training centers have begun using simulators in response to concerns regarding the animals' welfare. The American Heart Association neither endorses nor requires the use of animals in intubation training. =See also= * Advanced Pediatric Life Support (APLS) * Advanced cardiac life support, Advanced Cardiac Life Support (ACLS) * Neonatal Resuscitation Program (NRP) =References= =External links=American Heart Association
Pediatric Advanced Life Support Course -- PALS
{{Emergency medicine Medical credentials Emergency medicine courses Emergency life support Pediatrics